Could getting more high-quality sleep protect the brain?
Sleep is a hot commodity nowadays. More than 60 percent of Americans report their sleep needs aren't being met during a typical week. Illness, psychological distress, and medication can all interfere with adequate sleep. Add to that the normal physiological changes of the aging brain, and it's no wonder that older adults commonly complain of insomnia.
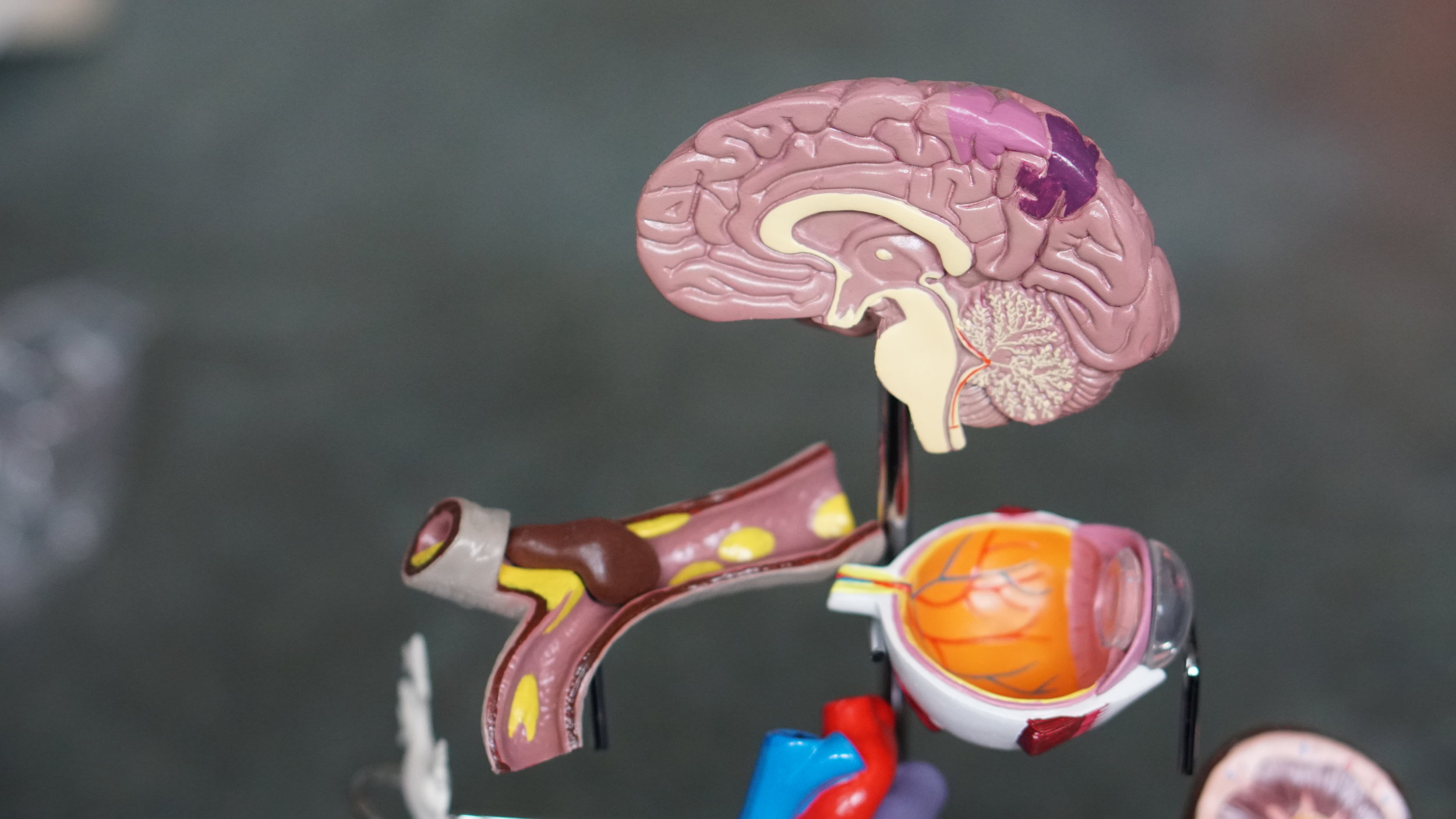
In mice, cerebrospinal fluid flows faster during sleep (left) than waking (right). (Istockphoto/Kali Nine LLC)
In mice, cerebrospinal fluid flows faster during sleep (left) than waking (right). (Istockphoto/Kali Nine LLC)
"Data show that older people tend to wake earlier and can't fall back to sleep, so they feel tired during the day," explains Brendan Lucey, M.D., instructor in the department of neurology at Washington University Sleep Medicine Center in St. Louis, MO, and member of the American Academy of Neurology (AAN). "We're just not sure why," he says.
Recent research suggests ongoing sleep deficits could take a considerable toll on the brain. Experts agree quality sleep is critical to cognitive function, especially in the short term. Studies show sleep deprivation hinders learning, impairs cognitive performance, and slows reaction time—like being intoxicated but without the buzz. Scientists recently discovered that sleep and memory storage are inextricably linked as well. Now, they are wondering whether poor sleep contributes to neurodegenerative diseases and cognitive decline.
The Waking Brain
Recently, scientists have started to link longer waking time with increased risk of cognitive impairment and a higher risk of developing Alzheimer's disease (AD). In a 2009 study of mice published in the journal Science, researchers found that sleep deprivation increases the concentration of harmful plaques in the brain. Other studies suggest that greater synaptic activity (the result of signaling and communication between brain cells) leads to more deposition of beta-amyloid, the hallmark protein associated with AD, in the brain. And recent neuroimaging studies suggest that excessive neural activity, such as from lack of sleep, may contribute to the onset of AD.
"For a long time, scientists believed that people with dementia don't sleep well because their brains are adversely affected by neurodegenerative disease," says Adam Spira, Ph.D., assistant professor in the department of mental health at the Johns Hopkins Bloomberg School of Public Health in Baltimore, MD. "But within the last 10 years or so, researchers have begun pondering whether insomnia might also be a potential cause of cognitive decline rather than simply something that emerges as a result of a neurodegenerative disease."
In a recent study of 70 healthy adults, Dr. Spira and his team at Johns Hopkins Bloomberg School of Public Health found that shorter self-reported sleep duration and poorer sleep quality were associated with a greater beta-amyloid burden. Unfortunately, from the results of this study, researchers can't answer the chicken-or-egg question: does sleep disturbance or beta-amyloid deposition come first? Plus, the authors only assessed self-reported sleep.
"People's perception of how much they sleep doesn't necessarily line up with reality," says Dr. Spira. Still, the correlation between disturbed sleep and beta-amyloid was strong—a surprise, according to Dr. Spira, given the limitations of self-reports. Researchers hope studies using objective measures of sleep will further explore whether poor sleep contributes to AD. In the meantime, scientists are left wondering how the two are related.
"We know aging is associated with sleep problems, and we know AD is associated with aging, but that doesn't mean the two are directly related," says David Knopman, M.D., professor of neurology at Mayo Clinic in Rochester Minnesota, deputy editor of the AAN's medical journal Neurology, and Fellow of the AAN. "That's the real pitfall here. Maybe disrupted sleep has nothing to do with AD, maybe it promotes some of the changes with AD, or maybe it's the reverse, that early AD changes alter sleep patterns. We don't know."
While this particular study doesn't prove a causal link, it does raise important questions about the role of sleep in the onset and progression of cognitive disease, and the mechanisms linking sleep-wake patterns and beta-amyloid burden. Other studies may answer these questions.
The Sleeping Brain
For centuries scientists and philosophers have debated what our brains do during sleep. Now, for the first time, researchers have solid evidence that a good night's sleep may literally clear the mind. In a study published in the journal Science, researchers found that the space surrounding brain cells—called the interstitial space—may increase during sleep, allowing the brain to flush out toxins that build up during waking hours. Previous research shows that proteins linked to neurodegenerative diseases, including beta-amyloid, build up in the interstitial space.
According to Dr. Spira, these findings provide a potential mechanism for the link between poor quality sleep and greater cognitive impairment. "It isn't a mechanism we imagined, but it's an intriguing and plausible explanation for what we saw," he says.
For the study, researchers injected dye into the cerebrospinal fluid (CSF) of mice and watched it flow through their brains while simultaneously monitoring electrical brain activity. (CSF is a clear fluid that bathes and cushions the brain and spinal cord; it is continuously produced and reabsorbed.) The dye flowed rapidly when the mice were asleep or anesthetized, but slowed to a sludge-like crawl when the mice were awake.
These same researchers also injected mice with labeled beta-amyloid and measured how long it lasted in their brains when they were awake or asleep. The results: interstitial space volume increased by 60 percent when the mice were asleep. In addition, toxic waste products, including beta-amyloid, disappeared at twice the rate in the brains of sleeping mice compared to those who were awake.
"The restorative function of sleep may be due to the switching of the brain into a state that facilitates the clearance of waste products that accumulate during wakefulness," says Rashid Deane, Ph.D., research professor in the department of neurosurgery's Center for Translational Neuromedicine at the University of Rochester Medical Center in New York. So perhaps there's not only less production of beta-amyloid during sleep, but more clearance as well.
Brain cells are highly sensitive to their environment. Toxins can interfere with nerve function and damage cells, so it's essential to quickly and efficiently remove waste products from the interstitial space. Yet, unlike every other organ in the body, the brain doesn't have a conventional lymphatic system to flush out waste products, explains Dr. Knopman. Instead, CSF recirculates through the brain, interchanging with interstitial fluid and removing toxic proteins, including beta-amyloid.
This plumbing system in the brain, which Dr. Deane's team has dubbed the glymphatic system, offers a potential solution to a mystery that has baffled brain researchers: how does the brain get rid of waste without the help of a lymphatic system?
"CSF is produced in the middle of the brain," explains Dr. Deane. "It flows over the brain along the blood vessels, percolates through the brain tissue between cells, and then finds its way out through the venous part of the vascular system." A bonus: in the flushing process, the brain may not only get rid of waste products but also may take up beneficial products.
When you host a party, you don't begin the process of cleaning up until after the guests head home. Brain cells operate similarly. When they're busy working and supporting normal function, they are not clearing material. During the sleep phase, they switch roles and get rid of waste products.
Previous research seems to support these findings. A 2009 study, also published in Science, reported that the amount of beta-amyloid found in the interstitial fluid of a mouse model of AD increased markedly during periods of sleep deprivation. And a 2012 study, published in the medical journal Archives of Neurology, showed that beta-amyloid levels in the spinal fluid of humans rose during waking hours and fell during sleep—a pattern that was more pronounced in healthy young people.
The Protected Brain
This growing body of research not only reaffirms the importance of sleep; it also hints at potential new strategies for slowing the onset and progression of AD and cognitive impairment.
"Over the last decade, researchers have sort of flipped the problem on its head, thinking about sleep disturbance as a modifiable risk factor for poor cognitive and neurologic outcomes," says Dr. Spira. In fact, several studies have looked at the link between sleep disturbance and cognitive decline—not just limited to insomnia, sleep duration, or sleep fragmentation, but also looking at sleep-disordered breathing, a condition characterized by abnormal breathing patterns during sleep that affects up to 60 percent of older adults. (For more Neurology Now coverage of sleep, including the cognitive effects of sleep-disordered breathing—such as due to obstructive sleep apnea—read more.)
A study of nearly 300 women published in Journal of the American Medical Association, for example, found that among older women, sleep-disordered breathing was associated with developing cognitive impairment. Other studies suggest that better sleep mitigates the effects of the gene apolipoprotein E e4 (APOE4), a common and well-established risk factor for AD.
"This could be a tremendous opportunity for prevention if there were in fact a causal link between disturbed sleep and AD or other forms of dementia," says Dr. Spira. "Given the significant increase of AD we're facing as a society, these results should encourage neurologists to take sleep seriously and not dismiss disturbed sleep as a normal part of aging."
AD is the most common form of dementing illness, and almost half of older adults report insomnia symptoms. Since late-life sleep disturbance is treatable, interventions to improve or maintain healthy sleep may help prevent or slow AD—or at least keep people with dementia as sharp as possible given the limitations of their illness. That's especially important because few effective treatments exist for cognitive impairment, dementia, and AD. Right now, our best tool may be to delay the onset of these conditions as long as possible.
"It's not clear that better sleep will have a dramatic impact on the risk of getting AD, but it certainly can have an impact on a day-to-day basis of how sharp you are cognitively," says Dr. Knopman. "Whatever its long-term effects might be, good sleep hygiene has obvious benefits the next day, so there's really no downside to maintaining good sleep."